The Pharma Legal Handbook: Japan
 The Pharma Legal Handbook: Japan answers essential questions about the legal and regulatory environment for pharmaceuticals in Japan. It is a must-have for any company operating in the country or looking to enter the market.
The Pharma Legal Handbook: Japan answers essential questions about the legal and regulatory environment for pharmaceuticals in Japan. It is a must-have for any company operating in the country or looking to enter the market.
Prepared in association with Nishimura & Asahi, the largest international law firm in Japan, it should answer any questions linked to regulation, pricing, clinical and preclinical trials, marketing, manufacturing, trademarks and patents.
February 2022
1. Biosimilars & Biologics: Japan
The key facts about biosimilars and biologics in Japan. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here.
1. Are biosimilar medicines considered the same as generic medicines in your country?
A biosimilar medicine is differentiated from a generic medicine to the extent that final biosimilar products may differ from the original product, depending on the manufacturing process. This is because the production of biosimilars is much more complicated, due to the complex molecular structure and unique manufacturing processes for biopharmaceuticals; on the other hand, producing generic medicines is not difficult because ordinary pharmaceuticals have simple and stable low-molecular compounds. This means an authorization for biosimilars does not constitute evidence of pharmaceutical equivalence, bioequivalence, or clinical equivalence to the original (preceding) biopharmaceuticals.
2. Are all biologic medicines, including biosimilar medicines, patentable in your country?
Yes, as long as the biologic medicine meets the general requirements of the Patent Act, its patentability is assured; in Japan, the patentability of biologic medicines is not specifically provided for in the act and other laws.
In this regard, Japan has not yet established a statutory system that coordinates the relationship between market approval for generic medicines or biosimilar medicines and the patent status of their branded original, such as a patent linkage system provided in the Drug Price Competition and Patent Term Restoration Act (well known as the Hatch-Waxman Act) or a patent dance system provided in the Biologics Price Competition and Innovation Act of 2009 (the “BPCIA”) in the United States. Though, as for generic medicines, a similar system has been put into practice at the governmental notification level. Under this coordination system, companies cannot obtain marketing approval for a generic medicine prior to the expiration of the patent term on the branded equivalent.
However, it is uncertain whether the word “generic medicine” in the notification includes biosimilar medicines. This suggests that it is possible that biosimilar medicines will not be treated in the same way as generic medicines, resulting in a situation where biosimilar medicines cannot acquire linkage protection. Therefore, the situation surrounding the patentability of biologic medicines is significantly different from other countries which have particular biopharmaceutical-protection systems, such as the BPCIA in the United States.
3. Is there a specific regulatory framework for the marketing authorization of biosimilar medicines in your country? If yes, what is the regulatory framework for the authorization of biosimilar medicines?
No. Refer to Question 2 with regard to the relationship between market approval for a biosimilar medicine and the patent status of its branded original.
4. What kind of data package is needed to obtain approval for a biosimilar drug? Is this any different to the requirements for the original Biologics drug?
Under the PMD Act, which establishes the need for market approval, there is no difference between the approval requirements for biosimilar drugs and those for other drugs. However, in many cases, it is difficult to prove that the active ingredients in the original Biologics drug are identical to those in its biosimilars, so it is thought that the same approval approach used for generic products cannot be applied to biosimilars.
Given this situation, the MHLW specifically issued a notification and guideline for market approvals for biosimilars. According to this documentation, the essential data required to obtain approval for a biosimilar drug are (1) data detailing the origin or history of discovery and usage status in foreign countries; (2) data detailing the manufacturing method, standards, test methods, etc.; (3) data detailing stability; (4) data detailing pharmacological action; (5) data detailing toxicity; and (6) data detailing the results of clinical studies. In addition to these data, depending on the nature of the biosimilar product, other data may be required.
5. What are the requirements for the choice of the reference comparator product?
According to the MHLW’s guideline, the reference product to which a biosimilar should be compared is a biologic drug that has been already authorized on the basis of a complete data package in Japan. Another biosimilar can never be used as a reference product, throughout the entire duration of the biosimilar development period (including the quality development period, non-clinical development period, and clinical development period).
6. Can the comparator product be sourced from another regulatory jurisdiction? If yes, what are the data needed to support this approach?
No. As mentioned in the response to Question 5, under the MHLW’s guideline, the reference comparator product must be a drug already authorized in Japan.
7. How are the prices of biosimilar medicines regulated? Is this any different from the requirements for the original Biologics drug?
In Japan, it is typically expected that drugs will be used under the auspices of the national health insurance system. The Japanese government determines the price of medicines by using a model established pursuant to the national health insurance pricing system.
The price of a new biosimilar medicine is generally determined by multiplying the standard price (which is calculated based on the price of the most similar drug to the biosimilar medicine) by 70%. However, for internal medicines, when the brand number of the same kind of biosimilar product (limited to those with similar efficacy and effect to the new biosimilar product) exceeds 10, the new biosimilar medicine’s price is determined by multiplying the standard price (as calculated the same above) by 60%. Exceptionally, based on the results of clinical trials, it may be possible to add a 10% premium (at most) to the price of a new biosimilar medicine.
8. What is the reimbursement policy for biosimilar medicine? Is this any different from the requirements for the original Biologic drug?
Biosimilar medicines are reimbursed under the National Health Insurance system in the same manner as other drugs. There is no special reimbursement procedure for biosimilar medicines.
In this regard, the Japanese government has promoted the development and use of biosimilars, and introduced special treatment regarding self-injection of biosimilars by patients, under which a certain price is added to self-injection instruction management charges when biosimilars are prescribed with the patient’s consent. Please note that this treatment is one kind of reimbursement (medical fee) revision under the National Health Insurance system, notwithstanding the medicine price decision itself, based on the PMD Act. This treatment has been in force since April 1, 2020.
9. Does biosimilar competition impact the reimbursement policy of the originator reference products?
Yes. The Japanese government has promoted biosimilars, which means there may be a strong competitive effect on the existing biopharmaceuticals market. This is mainly due to the fact that they are less expensive (as mentioned in the response to Question 7) and in light of the reimbursement policies (as mentioned in the response to Question 8). The Japanese government is planning other strategies to accelerate the introduction of biosimilars into medical practice in Japan, so it is necessary to continue monitoring these movements.
10. What is the legal framework for biosimilar medicines prescribing (clinical decision maker) and dispensing (pharmacy level, hospital or retail)? Is this any different to the requirements for the original Biologics drug?
There is no particular legal framework for prescribing biosimilars.
11. Is the system considering physician-led switching and/or pharmacy-level substitution (without involvement of the clinical decision maker)?
Switching patients from biologics to biosimilars is fundamentally permitted for doctors. There is no clear rule banning pharmacists from changing biologics to biosimilars, but it is not recommended that pharmacists do so, in medical practice.
12. What are the post – authorisation requirements (including pharmacovigilance, risk management plans, post-approval studies) for biosimilar medicines? Is this any different to the requirements for the original Biologics drug?
Manufacturers must set up methods for post-marketing safety control for pharmaceuticals (referring to collecting and reviewing matters related to quality, efficacy and safety, and other information necessary for the appropriate use thereof, and necessary measures based on the results), and those methods have to comply with the standards specified by order of the MHLW. This rule also applies to biosimilar medicines, but if their efficacy and safety are assured by the original biologics drugs, they are exempt from this rule, including post-marketing safety control research.
However, a guideline by the MHLW (referred to in the response to Q126) suggests that manufacturers should research the safety profiles of biosimilar medicines. In terms of this post-marketing safety control research, the guideline also requires that manufacturers anticipate risks that could not be sufficiently evaluated by the equivalence/homogeneity evaluation during the development stage, formulate an appropriately designed post-marketing surveillance plan based on those risks, and submit it to the authority when applying for approval. In addition, the guideline provides that the results of such a post-marketing surveillance plan should be delivered to the authority by the appropriate time after approval of the biosimilars.
13. Are there specific policies and requirements for labelling biosimilar medicines in the event of second medical use patents? Is this any different from the requirements for the original Biologic drug?
No. There are no specific policies and requirements regarding the labelling of biosimilar drugs in the case of a second medical use patent.
14. Have there been any significant legal/judicial developments in relation to biosimilars in your country? (Including but not limited to IP, procurement, competition, misleading information campaign, access to reference comparator product)
Yes. In recent years, the Japanese government has promoted biosimilars in some way. Please refer to Question 7 and Question 9.
15. Are there proposals for reform or significant change to the legal, regulatory, procurement of biosimilars? If yes, when are they likely to come into force?
Yes. In recent years, the Japanese government has promoted biosimilars in some way. Please refer to Question 7 and Question 9.
————————————————-
- The the Minister of Health, Labour and Welfare (“MHLW”) as the Japanese authority issued a notification detailing this matter: https://www.mhlw.go.jp/web/t_doc?dataId=00tb5511&dataType=1&pageNo=1
- http://www.nihs.go.jp/dbcb/TEXT/yakusyokuhatu-0304004.pdf
https://www.pmda.go.jp/files/000206248.pdf -
Please refer to the detailed calculation method; online: https://www.mhlw.go.jp/content/000497468.pdf
Also from this Legal Handbook
2. Localization: Japan
The key facts about localization in Japan. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
1. Are there any rules or regulations requiring and/or encouraging localization in your country? What is the legal framework defining these localization rules and policies?
No, there are no rules or regulations requiring and/or encouraging localization in Japan. This means that the decision about whether to import and sell pharmaceuticals made in foreign countries or to sell domestically manufactured pharmaceuticals generally is left to the distributors’ individual judgment.
Please note that no person other than one who has obtained marketing authorisation from the MHLW may engage in the business of marketing pharmaceuticals in Japan. This regulation is set forth in the PMD Act. In relation to obtaining such a license, this law requires that the applicant should have methods for quality control for pharmaceuticals which comply with the standards specified by the Order of the MHLW for the purpose of obtaining such license; one such order is the Ministerial Ordinance on Standards for Quality Assurance for Drugs, Quasi-drugs, Cosmetics and Medical Devices. According to this order, a marketing authorisation holder shall have a person, designated beforehand, in its quality assurance department or manufacturing department who evaluates the results of the manufacturing control and quality control and makes decisions concerning the market release for each lot. This rule applies to distributors (marketing authorisation holders) who sell pharmaceuticals imported from foreign countries.
2. Have there been any recent significant changes involving localization rules? If yes, when did they take place and what did they involve?
N/A.
3. Is the process of obtaining a marketing authorization impacted by localization policies in your country? If yes, how so (what are the incentives received or the requirements)?
N/A.
4. Is the pricing process for pharmaceutical products impacted by localization policies in your country? If yes, how so (what are the incentives received or the requirements)?
N/A.
5. Is the reimbursement of pharmaceutical products impacted by localization policies in your country? If yes, how so (what are the incentives received or the requirements)?
N/A.
6. Is the access to public or public tenders of pharmaceutical products impacted by localization policies in your country? If yes, how so (what are the incentives received or the requirements)?
N/A
7. Are import tariffs, importation and/or exportation permits, trade and/or taxation of pharmaceutical products impacted by localization policies in your country? If yes, how so?
N/A.
8. Are there any other incentives or advantages offered by the current local localization rules in your country? If yes, what are they?
N/A.
9. Are there discussions about the possibility of implementing localization policies in your country? If yes, what are the proposed reforms and when should they come into place?
Currently, there are no discussions in progress concerning the possibility of implementing localization policies in Japan.
Also from this Legal Handbook
3. Cannabinoid Drugs, Medicinal Cannabis and Opioid Drugs: Japan
Keen to learn more about cannabinoid drugs, medicinal cannabis and opioid drugs in Japan? Read on! Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
Cannabinoid Drugs
1. Are Cannabinoid Drugs authorized in your country?
No. In Japan, the utilisation of cannabis (all kinds) is severely restricted by two acts.
The first is the Cannabis Control Act, under which “Cannabis” is defined as the cannabis plant (Cannabis Sativa L.) and its products; provided, however, that the grown stalk of the cannabis plant and its products (excluding resin) and the seed of the cannabis plant and its products are excluded from this definition. The Cannabis Control Act states that any person who is not a cannabis handler (the term “cannabis handler” includes cannabis researchers) must not possess, cultivate, receive, or transfer cannabis, or make research use of it. Furthermore, it is prohibited for any person to perform any treatment with medicines manufactured from cannabis, to distribute cannabis for treatment purposes, and/or to receive treatment with any medicines manufactured from cannabis.
It is worth noting that this act does not prohibit the act of using cannabis (including the act of smoking cannabis) per se. This is due to the fact that before World War II, cannabis grass was widely cultivated in Japan, and even today cannabis grass is grown in some parts of Japan for its fibre, which is used in clothing; this leads to the possibility that farmers accidentally might inhale cannabis components dispersed into the air when they cut cannabis grass.
The second act is the Narcotics and Psychotropics Control Act. This Act aims to prevent any health and sanitation hazards caused by the abuse of narcotics (and psychotropics). Cannabis is not expressly covered in the act, but tetrahydrocannabinol (THC), a major cannabinoid present in cannabis, is regulated as a narcotic under the act, provided it is chemically synthesized.
2. What are the regulatory authorities with jurisdiction over Cannabinoid Drugs?
N/A.
3. Is there a specific regulatory framework for the authorization, pricing, and reimbursement of Cannabinoid Drugs?
N/A.
4. Which are the cannabinoid drugs that have received market approval to date?
N/A.
5. Who can prescribe Cannabinoid Drugs?
N/A.
6. Is there a list of doctors authorized to prescribe Cannabinoid Drugs?
N/A.
7. What approvals or notifications are required to prescribe Cannabinoid Drugs?
N/A.
8. Which organizations are authorized to sell/distribute Cannabinoid Drugs available?
N/A.
9. Is there a list of retailers/distributors authorized to sell Cannabinoid Drugs?
N/A.
10. Are there proposals for reform or significant change to the regulation of Cannabinoid Drugs?
In June 2021, after considering the recent trends in other countries and the medical usefulness of cannabis, a study council organised by the MHLW proposed that the production and application of medicines made from cannabis should be made possible.
11. When are they likely to come into force?
Despite the aforementioned proposal, at present there is no active debate in the Japanese Parliament concerning the production and sale of cannabis-based medicines.
Medicinal Cannabis
12. Is Medicinal Cannabis authorized in the country?
Any use of all types of cannabis is banned by the Cannabis Control Act, regardless of the name of the product or the purpose of its use, unless it is made from grown stalks or seeds of the cannabis plant (refer to Q68). One notable exception is cannabis researchers (persons who receive licenses from a prefectural governor and cultivate cannabis plants for the purpose of researching cannabis). Cannabis researchers are permitted to possess, cultivate, receive, and/or transfer cannabis, and to make research use of it. Additionally, cannabis researchers are allowed to import cannabis to Japan only if they satisfy certain requirements (refer to Q82).
13. What are the regulatory authorities with jurisdiction over Medicinal Cannabis?
N/A.
14. What is the regulatory framework for the authorization, pricing, and reimbursement of Medicinal Cannabis?
N/A.
15. How is the production and import of Medicinal Cannabis regulated and by which agencies/authorities?
Under the Cannabis Control Act, the import of cannabis to Japan is prohibited. However, cannabis researchers who have received authorisation from the MHLW to import cannabis are excluded from this prohibition.
16. What approval or notifications are necessary to produce or import Medicinal Cannabis?
Registration as a cannabis researcher is the first requirement. Moreover, to import cannabis, it is also necessary for the relevant cannabis researchers to receive authorization from the MHLW.
17. What is the regulatory framework for the marketing and distribution of Medicinal Cannabis?
N/A.
18. How can patients obtain Medicinal Cannabis?
N/A.
19. Who can prescribe Medicinal Cannabis?
N/A.
20. Is there a list of doctors authorized to prescribe Medicinal Cannabis?
N/A.
21. What approvals or notifications are required to prescribe Medicinal Cannabis?
N/A.
22. Where is Medicinal Cannabis available?
N/A.
23. Is there a list of retailers authorized to sell Medicinal Cannabis?
N/A.
24. Are there proposals for reform or significant change to the regulation of Medicinal Cannabis?
N/A.
Opioid Drugs
25. Are Opioid Drugs authorized in your country?
Some Opioid Drugs are authorized for sale as legitimate pharmaceutical products, based on the PMD Act. Additionally, in Japan, most opioid drugs are treated as narcotics and regulated under the Narcotics and Psychotropics Control Act. Therefore, as long as the requirements are satisfied, Opioid Drugs may be medically prescribed and distributed in compliance with the stringent regulatory framework established by those acts and the related regulations.
26. What are the regulatory authorities with jurisdiction over Opioid Drugs?
The central authority with jurisdiction over Opioid Drugs is the MHLW. Prefectural governors and the heads of the respective Regional Bureaus of Health and Welfare are also involved in issuing some licenses.
27. Is there a specific regulatory framework for the authorization, pricing, and reimbursement of Opioid Drugs?
Opioid Drugs can be authorized for sale in Japan once the relevant review process has been completed successfully, in accordance with the applicable requirements in the PMD Act and related regulations.
There is no specific regulatory framework for the pricing of and reimbursement for Opioid Drugs in Japan.
28. Which are the Opioid drugs that have received market approval to date?
Some Opioid Drugs already have received market approval. They include morphine, oxycodone, fentanyl, methadone, hydromorphone, codeine, and dihydrocodeine. Please note that these Opioid Drugs are designated as narcotics under the Narcotics and Psychotropics Control Act.
29. Who can prescribe Opioid Drugs?
Essentially, it is prohibited for anyone who is not a Person Licensed to Administer Narcotics to administer a narcotic, deliver a person a narcotic to administer, or deliver a prescription for a narcotic. A “Person Licensed to Administer Narcotics” means a person who has been licensed by the prefectural governor to administer narcotics, deliver a person a narcotic to administer, or deliver prescriptions for a narcotic in the course of business and as treatment for an illness. It is not permissible for a person other than a physician, dentist, or veterinarian to obtain licensing as a Person Licensed to Administer Narcotics.
30. Is there a list of entities authorized to prescribe Opioid Drugs?
No. There is no public list of licensed doctors authorized to prescribe Opioid Drugs as a Person Licensed to Administer Narcotics in Japan.
31. What approvals or notifications are required to prescribe Opioid Drugs?
Persons Licensed to Administer Narcotics may prescribe Opioid Drugs without additional approval or notification. Please note that a Person Licensed to Administer Narcotics must not administer a narcotic, deliver a narcotic to administer, or deliver a prescription for a narcotic for any purpose other than treatment for an illness.
32. Which organizations are authorized to sell/distribute Opioid Drugs available?
Essentially, it is prohibited for anyone who is not a Commercial Narcotics Handler to sell/distribute a narcotic. A “Commercial Narcotics Handler” means a Narcotics Importer, Narcotics Exporter, Narcotics Manufacturer, Formulator of Narcotic Pharmaceuticals, Manufacturer of Exempt Narcotics, Primary Wholesaler of Narcotics, Narcotics Wholesaler, or Narcotics Retailer.
33. Is there a list of retailers/distributors authorized to sell Opioid Drugs?
No. There is no public list of licensed retailers/distributors authorized to sell Opioid Drugs in Japan.
34. Are there proposals for reform or significant change to the regulation of Opioid Drugs?
No. There is currently no noticeable movement for reform of or significant changes to the regulation of Opioid Drugs.
35. When are they likely to come into force?
N/A.
Also from this Legal Handbook
4. Orphan Drugs & Rare Diseases: Japan
The ins and outs of orphan drugs & rare diseases in Japan. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
1. What is the definition of Rare Diseases in your country?
In Japan, there is no fixed definition for Rare Diseases, although the concept is included in the definition of Orphan Drugs (refer to Q104). It should be noted that our country has a system to deal with diseases designated as “Intractable Diseases,” the definition of which is provided in the Act on Medical Care for Intractable Disease Patient (the “Intractable Disease Act”), but the range and definition of Rare Diseases do not necessarily correspond to those of Intractable Diseases.
2. Does the designation of ‘Orphan Drug’ exist in your country? (Does it correspond with the definition of Rare Diseases?)
An “Orphan Drug” is defined as a pharmaceutical designated as such by the MHLW under the PMD Act. More specifically, the MHLW can designate a pharmaceutical as an Orphan Drug when all of the following requirements are satisfied: (i) the number of patients who need the drug is less than 50,000; (ii) there is no alternative drug, and the drug has particularly excellent efficacy or safety; and (iii) the manufacturers have a possible and reasonable development plan for the drug. As an exception to requirement (i), if a disease falls within a category provided in the Intractable Disease Act, the number of patients may be changed to comply with the relevant provision of that act.
3. What is the regulatory framework for the authorization of an Orphan Drug? (Is this regulatory framework based on Rare Disease status or can it alternatively be based on Orphan Drug foreign status?)
Designation of an Orphan Drug does not immediately lead to approval (authorization) for the manufacture and sale of the drug. The process for Orphan Drug authorization is essentially the same as that for ordinary drugs. However, certain priority treatment is given during the approval review for an Orphan Drug, for purposes of expediting its development. More precisely, if a drug is designated as an Orphan Drug, its approval review is prioritized (in terms of time) over an examination or investigation into other pharmaceuticals. The Japanese regulatory framework does not consider an Orphan Drug’s foreign status.
4. Does your country have provisions for relaxed clinical trial/scientific evidence requirements in respect of Orphan Drugs as compared to other drugs?
No. Currently, Japan does not have any provisions for relaxed clinical trial/scientific evidence requirements with respect to Orphan Drugs as compared with other drugs.
5. Is there an expedited pathway for Orphan Drugs?
As stated in Q104, if a drug is designated as an Orphan Drug, a priority review process is applicable to the approval (authorization) of the manufacture and sale of the drug. To clarify, however, there is no expedited pathway for the designation of Orphan Drugs.
6. Are foreign marketing authorizations recognized in your jurisdiction for Orphan Drugs? If yes, marketing authorizations from which countries are recognized?
No foreign marketing authorizations are recognized for Orphan Drugs in Japan.
7. Can Orphan Drugs be reimbursed? If so, is there a specific reimbursement procedure for Orphan drugs?
Yes, Orphan Drugs are reimbursed under the National Health Insurance. However, there is no special reimbursement procedure for Orphan Drugs.
8. How are the prices of Orphan Drugs regulated?
In Japan, drugs are typically expected to be used under the auspices of the national health insurance system. The Japanese government determines the price of medicines by using a model established under the national health insurance pricing system. The prices of Orphan Drugs are regulated in the same manner as other drugs. However, under the pricing model, Orphan Drugs will normally receive an additional price. In addition, Orphan Drugs receive special treatment regarding price decisions, under which the prices of Orphan Drugs are exempt from periodic price cuts for a certain period of time.
9. In case of reference price based on a basket of countries, what countries are included?
When determining the price of a new drug that already been made available for sale in countries other than Japan, the government adjusts the price so that there is no significant price difference between Japan and certain other countries. The countries used for comparison are the United States, the United Kingdom, Germany, and France.
10. Have there been any significant legal/judicial developments in relation to Orphan Drugs in your country?
No. There have not been any recent significant legal/judicial developments relating to Orphan Drugs in Japan.
11. Are there proposals for reform or significant change to the regulation of Orphan Drugs? If yes, when are they likely to come into force?
No. There is currently no noticeable movement for reform of or significant changes to the regulation of Orphan Drugs.
Also from this Legal Handbook
5. Regulatory Reforms: Japan
The key facts about regulatory reforms in Japanese Pharma. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
1. Are there proposals for reform or significant change to the healthcare system?
No proposal is pending for significant reform or change to the healthcare system in Japan. However, there are small changes every year. For example, there have been changes due to technology, telemedicine, apps as a medical device, and enactment of the Healthcare Big Data Act, and changes due to compliance issues, promotion guidelines, monitoring, and enactment of the Clinical Trials Act.
2. When are they likely to come into force?
Small changes and developments occur on an ongoing basis.
Click the following links to read more legal articles from Japan:
- Regulatory Pricing and Reimbursement Overview
- Preclinical and Clinical Trial Requirements
- Marketing, Manufacturing, Packaging & Labeling, Advertising
- Traditional Medicines and OTC Products
- Product Liability
- Patents & Trademarks
- Regulatory Reform
Also from this Legal Handbook
6. Patents and Trademarks: Japan
The legal framework for patents and trademarks in Japanese Pharma. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
1. What are the basic requirements to obtain patent and trademark protection?
The Patent Act states that an invention must be novel, non-obvious, and have industrial applicability. The Trademark Act allows registration of any trademark unless the mark is the same as or similar to another registered mark or otherwise prohibited under the Act. On top of the Trademark Act restrictions, there is a special restriction for medicine to avoid confusion among medicines.
2. What agencies or bodies regulate patents and trademarks?
The Japan Patent Office (the “JPO”) regulates both patents and trademarks.
3. What products, substances, and processes can be protected by patents or trademarks and what types cannot be protected?
For patents, basically any novel, non-obvious substances and processes with industrial applications can be protected. However, under the Japanese Patent Act, medical treatments and related practices are not approved for patents. In general, no patents can be granted for any method of operating on, treating, or diagnosing human bodies. This regulation is similar to Article 53(c) of the European Patent Convention. Although this regulation had been controversial, especially with regard to regenerative medicine technologies and gene therapy, a revision to the relevant guideline in 2003 made some of those technologies distinct from medical treatments and subject to patenting. However, it is worth noting that regenerative medicine technologies and gene therapy are also problematic from a moral perspective (public order and decency). For instance, a technology to create human embryonic stem cells has the former issue, while a genome editing technology (such as CRISPR-Cas9) applied to germ cells (including fertilised human embryos) has implications for the latter. Discussion of these points have intensified in recent years (see a parallel discussion in Article 53(a) of the European Patent Convention).
In the trademark area, the name of a medicine that would create consumer confusion with regard to other medicines will not be approved, even if a trademark on the name is granted under the Trademark Act.
4. How can patents and trademarks be revoked?
Any interested party may make a claim for invalidation of patents or trademarks via a request to the JPO. The JPO will decide whether or not a patent or a trademark should be revoked, as the evaluator in the first instance. The second instance evaluator of an invalidation request is the Intellectual Property High Court of Japan, which is a branch of the Tokyo High Court. If the litigants are unsatisfied with that judgement, they can appeal to the Supreme Court of Japan.
5. Are foreign patents and trademarks recognized and under what circumstances?
No such recognition is granted.
A foreign patent applicant can submit an international application to its home country under the Patent Cooperation Treaty (the “PCT”) and can include Japan as one of the target countries in that application. However, even in such cases, whether a patent will be granted for the relevant invention ultimately is left to the discretion of the JPO, after a substantive examination. Apart from the PCT and the Paris Convention for the Protection of Industrial Property (which is a fundamental treaty for industrial property), Japan is neither a member of any international patent application system (e.g., European patent under the European Patent Convention) nor a member of any unified international patent framework (e.g., European patent with unitary effect under the Regulation (EU) No 1257/2012).
6. Are there any non-patent/trademark barriers to competition to protect medicines or devices?
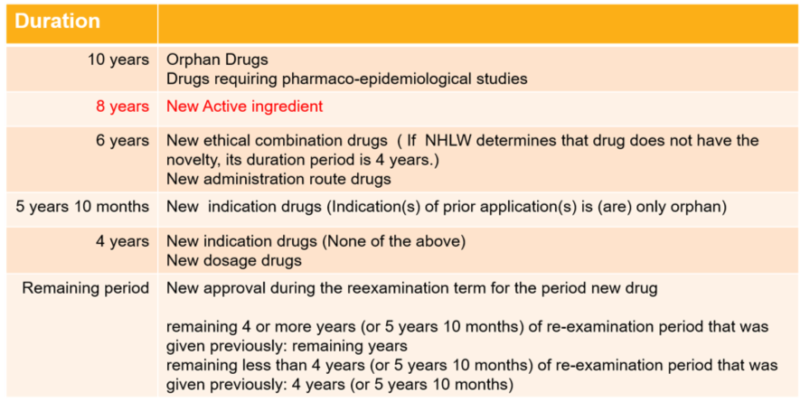
The PMD Act creates a Re-examination System, and provides for a certain Re-examination Period when a new medicine is approved, or in other cases set forth in the list below.
The Re-examination Period may be extended for a certain length of time, not to exceed ten years. The purpose of the Re-examination Period is to obtain safety and efficacy evidence in the real healthcare market. The MA holder must conduct research and trials pursuant to an agreement reached with the MHLW at the time of approval, including Post-Marketing Surveillance and gathering Drug Safety Information Data during the Re-examination Period. Then, after the relevant period, the MHLW will re-examine and approve the efficacy and safety of the medicine. Until the medicine is re-examined and approved, generic medicines cannot come into the market. In other words, in order to market generic medicines, it is a prerequisite that the Re-examination Period for the corresponding pioneer drug has been completed and that an evaluation of its efficacy and effectiveness has been established. Accordingly, the Re-examination Period works similar to Data Exclusivity in other jurisdictions.
7. Are there restrictions on the types of medicines or devices that can be granted patent and trademark protection?
No.
8. Must a patent or trademark license agreement with a foreign licensor be approved or accepted by any government or regulatory body?
No.
Click the following links to read more legal articles from Japan:
- Regulatory Pricing and Reimbursement Overview
- Preclinical and Clinical Trial Requirements
- Marketing, Manufacturing, Packaging & Labeling, Advertising
- Traditional Medicines and OTC Products
- Product Liability
- Patents & Trademarks
- Regulatory Reform
Also from this Legal Handbook
7. Product Liability: Japan
All legal aspects surrounding product liability in Japanese Pharma. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
1. What types of liability are recognized in your jurisdiction?
Contract liability and tort liability are the two basic forms of civil liability. In principle, tort liability requires intent or negligence. However, Japan has the Product Liability Law under which liability can arise even without negligence if a product is found to be defective.
2. How do these types of liabilities apply to the manufacturers of medicines and devices?
All of the foregoing types of liability apply to the manufacturers of medicines and medical devices.
3. Does potential liability extend to the manufacturer only or could claims extend to corporate executives, employees, and representatives?
In principle, product liability extends to the manufacturer. However, theoretically, a person who acted willfully or negligently may be liable under tort law.
4. How can a liability claim be brought?
Liability claims shall be brought in courts that have jurisdiction.
5. What defenses are available?
The plaintiff bears the burden of proof in the lawsuit, and any defense available under the rules of civil procedure is available to the defendant. Under the Product Liability Law, the defense of development risk is applicable to the defendant, but as a practical matter, the standard for establishing the defense of development risk is strict and not accepted by Japanese courts.
Click the following links to read more legal articles from Japan:
- Regulatory Pricing and Reimbursement Overview
- Preclinical and Clinical Trial Requirements
- Marketing, Manufacturing, Packaging & Labeling, Advertising
- Traditional Medicines and OTC Products
- Product Liability
- Patents & Trademarks
- Regulatory Reform
Also from this Legal Handbook
8. Traditional Medicines and OTC Products: Japan
A brief overview of the situation regarding traditional medicines and OTC products in Japan. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
1. What are the regulatory requirements for traditional, herbal, complementary, or alternative medicines and devices?
Traditional, herbal, complementary, and/or alternative medicines and devices are subject to the PMD Act.
2. Can these traditional, herbal, complementary, or alternative products be advertised directly to the public?
If the relevant traditional, herbal, complementary or alternative products are not prescription medicines, then they can be advertised directly to the public.
3. What health, advertising, and marketing claims may be made for traditional, herbal, complementary, or alternative products?
False, exaggerated, and misleading advertisements and off-label advertisements are prohibited; advertisements that cause fear are also prohibited.
4. What are the regulatory requirements for over-the-counter (non-prescription) medications?
Over-the-counter medications are governed by the PMD Act. OTC products are subject to Marketing Authorization approval, with less strict data requirements compared with prescription medicine, but the requirements vary depending on the nature of the product.
5. Are there any limitations on locations or channels through which OTC products may be sold?
OTC products can be sold at places where a pharmacist is available, such as pharmacies and drug stores. Basically, OTC products are categorized in one of three types. Type one can be sold only where a pharmacist is available. Categories two and three can be sold if a licensed person (non-pharmacist) is available. OTC products, other than special products, such as switch OTC products, can also be sold via the internet.
6. What health, advertising, and marketing claims may be made for OTC products?
False, exaggerated and misleading advertisements and off-label advertisements are prohibited; advertisements that cause fear are also prohibited.
7. Can OTC products be marketed or advertised directly to the public?
Yes.
8. What is the mechanism by which a prescription-only product can be converted to an OTC product?
Conversion of a prescription-only product to an OTC product is called “switch OTC.” A prescription-only product can be switched to OTC if the relevant product has been used in the market for a long time with no severe adverse events. Generally, switch OTC products are under strict control for three years after the switch, and cannot be sold via the internet during that time.
9. What are the requirements for the importation of either traditional medicines or OTC products?
There are no specific importation rules for traditional medicines or OTC products; they are subject to the same rules under the PMD Act.
Click the following links to read more legal articles from Japan:
- Regulatory Pricing and Reimbursement Overview
- Preclinical and Clinical Trial Requirements
- Marketing, Manufacturing, Packaging & Labeling, Advertising
- Traditional Medicines and OTC Products
- Product Liability
- Patents & Trademarks
- Regulatory Reform
Also from this Legal Handbook
9. Marketing, Manufacturing, Packaging & Labeling, Advertising: Japan
Marketing, manufacturing, packaging & labeling, advertising in Japanese Pharma – a comprehensive legal overview. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
1. What is the authorization process for the marketing of new drugs, biologics, medical devices, over-the-counter medications, and other medicinal products?
To obtain marketing authorization for new drugs, biologics, and medical devices, submission of an application to the PMDA is required, along with submission of the data from the clinical trial. Under certain conditions and pursuant to an agreement with the PMDA, an applicant may apply for marketing authorization without submitting the data from confirmatory clinical trials, on the condition that the efficacy and safety will be reconfirmed after marketing commences.
Authorization processes for over-the-counter (“OTC”) medications differ depending on the kind of the drug, i.e., new drug/new indication, switch OTC (see below) and other OTC products. New drug/new indication requires the same process as new prescription drugs. A drug used in the medical market as a prescription drug for a long time, the safety of which has been established, can be approved as an OTC product (“switch OTC”). Switch OTC applications are examined at the PMDA through consultation with the Central Pharmaceutical Affairs Council. Most OTC products are low risk and the active ingredients are the same as those used in the market for a long time. These are either examined by the local prefectural government or by the PMDA.
Under the PMD Act, some products are categorized as Quasi-drugs. These are examined either by the local prefectural government or by the PMDA.
2. What is the authorization process for the marketing of generic versions of these products?
The authorization process for the marketing of generic products is the same as that for new drugs, but for generic products, clinical trial data is not required; only stability test data and bioequivalence test data are required.
3. What are the typical fees for marketing approval?
Fees for a marketing authorization vary significantly, depending on the type of product. For example, the fee for a new, high-end drug product is approximately 50,000,000 yen, and the fee for a new high-end medical device is approximately 20,000,000 yen. In addition, consultation with the PMDA is required, and a consulting fee is charged in connection therewith.
4. What is the period of authorization and the renewal process?
There is no limit to the authorization period and thus, no renewal process.
5. What are the requirements, if any, for post-approval pharmacovigilance?
There are two rules relating to post-marketing surveillance (“PMS”). One is Good Post-marketing Study Practice (“GPSP”) and the other is Good Vigilance Practice (“GVP”). Pursuant to GPSP, the holder of the marketing authorization must conduct a treatment outcome study, a special treatment outcome study, and a post-marketing clinical trial. Pursuant to GVP, the holder of the marketing authorization must collect safety information and take action thereon and must conduct early post-marketing phase vigilance (“EPPV”), which involves surveillance for the first 6 months after starting sales in the market.
6. Are foreign marketing authorizations recognized?
Foreign marketing authorizations are recognized under the PMD Act. A foreign marketing authorization applicant has to designate a manufacturing/marketing business license holder in Japan. If the foreign marketing authorization is granted to a foreign company, then the designated manufacturing/marketing business license holder may manufacture and sell the authorized product.
7. Are parallel imports of medicines or devices allowed?
No.
8. What are the restrictions on marketing practices such as gifts, sponsorships, consultancy agreements, travel and entertainment, or other incentives for healthcare organizations and individual medical practitioners?
Incentives are strictly restricted under industry rules.
Japan has two pharmaceutical industry associations. One is the Japan Pharmaceutical Manufacturers Association (the “JPMA”) which is a member of the International Federation of Pharmaceutical Manufacturers & Associations (the “IFPMA”). The other is The Fair Trade Council of the Ethical Pharmaceutical Drugs Marketing Industry (the “FTC”). Both industry associations have rules regarding gifts and other incentives. The JPMA has basically the same rules as the IFPMA. The FTC is a Japan-specific organization established under the Act Against Unjustifiable Premiums and Misleading Representations, one of Japan’s antitrust laws. The FTC established the Fair Competition Code of Ethical Pharmaceutical Drugs (the “FCC”), and the FCC has detailed provisions relating to gifts and other incentives to healthcare organizations and individual medical practitioners.
The Medical Device industry has industry associations similar to the pharmaceutical industry, and similar rules apply.
9. How is the manufacturing of medicines and devices regulated and by which agencies?
Manufacturing of medicines and devices are regulated under the PMD Act, and the agencies are the local prefectural governments, the MHLW and the PMDA.
10. Are local manufacturing requirements compatible with Good Manufacturing Practices (GMPs) as defined by the U.S. Food & Drug Administration and/or the European Medicines Agency?
Yes. Japan is a member of PIC/S and has an MRA with the EU.
11. What is the inspection regime for manufacturing facilities?
Under the PMD Act, a manufacturer has an obligation to allow GMP Compliance Inspections by the local prefectural government or the PMDA at the time of examination of marketing authorization and every five years thereafter.
12. Are manufacturing facilities open for inspection by foreign inspectors or third-party inspectors as authorized by the FDA/EMA?
Yes.
13. What are the requirements for the storage, packaging, and handling of medicines and devices and their constituent components?
Storage, packaging, and handling of medicines and devices are governed by the PMD Act and regulations. Also, the MHLW announced a GDP Guideline in January 2019, which is harmonized with the PIC/S GDP Guideline. Thus, storage, packaging, and handling of medicines and devices now are harmonized with global standards.
14. What information must be included in medicine and device labeling?
The PMD Act provides the information to be included in labeling (package inserts). The MHLW has also issued package insert notifications and provided guidelines. According to the PMD Act, package inserts must include: the drug name(s), warnings, contraindications, composition and properties, indications and efficacy, usage and administration, usage notes (including adverse events, combination use, and use by pregnant women, children or senior people), and other information specified by law.
15. What additional information may be included in labeling and packaging?
What information “may” be included is not specified, but any false, exaggerated, or misleading information is prohibited from inclusion in labeling and packaging.
16. What items may not be included in labeling and packaging?
False or misleading information, indications and efficacy which have not been approved, and usage and administration or expiration information that may cause risks to health and hygiene may not be included.
17. What are the restrictions and requirements for the marketing and advertising of medicines and devices?
Under the PMD Act, false or exaggerated advertisements are prohibited, as is any advertisement performed before obtaining marketing authorization. Rules and guidelines relating to advertisements are issued by the healthcare authority, as well as promotion codes and other self-imposed rules created by industry associations.
18. Where can medicines and devices be sold or delivered? Can medicines and devices be sold or delivered via post?
Prescription medicines and devices are sold only at hospitals, clinics, and pharmacies, and only may be delivered by licensed organizations. Medicines can be delivered by post, to reduce waiting time at the pharmacy, if a pharmacist has given face to face medication instructions to the patient before dispensing and posting such medicines. In addition, medication instructions can be provided online under certain conditions.
19. What are the restrictions and requirements for electronic marketing and advertising via email, by Internet, social media, and other channels?
There are no specific restrictions and requirements for electronic marketing and advertisements for prescription medicines and medical devices. Therefore, the general legal framework applicable to advertisements for medicine and medical devices, and general electronic marketing and advertising rules apply.
20. May medicines and devices be advertised or sold directly to consumers?
No. Prescription medicines and/or prescription medical devices may not be advertised or sold directly to consumers.
21. How is compliance monitored?
Generally, the MHLW (Compliance and Narcotics Division) and the governments of each prefecture are in charge of compliance monitoring. In addition to this general monitoring, the MHLW has introduced special monitoring activities for advertisements of medicine (including oral promotions by sales reps) starting in 2017, and publishes a report every year.
22. What are the potential penalties for noncompliance?
Under the PMD Act, potential penalties are up to two years’ imprisonment or a fine of up to two million yen, or both. The two million yen fine may also be assessed against a company.
In addition, a surcharge equivalent to 4.5% of the amount of sales will be imposed on companies that engage in false or exaggerated advertising of pharmaceuticals, medical devices, etc., in a manner prohibited by the PMD Act.
Click the following links to read more legal articles from Japan:
- Regulatory Pricing and Reimbursement Overview
- Preclinical and Clinical Trial Requirements
- Marketing, Manufacturing, Packaging & Labeling, Advertising
- Traditional Medicines and OTC Products
- Product Liability
- Patents & Trademarks
- Regulatory Reform
Also from this Legal Handbook
10. Preclinical & Clinical Trial Requirements: Japan
The low-down on the situation regarding preclinical & clinical trial requirements in Japanese Pharma. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
1. Are clinical trials required to be conducted locally as a condition (stated or implicit) for marketing approval?
Generally, under the PMD Act, clinical trials relating to applications for marketing authorization approval must be conducted locally. However, data from foreign clinical trials can be used as a reference, depending on the conditions of those foreign clinical trials.
In case of additional indications, public knowledge-based applications are allowed, if foreign countries that have a harmonized approval system have approved a product and have substantial experience with its use. In this exceptional case, local clinical trials are not required.
2. How are clinical trials funded?
Clinical trials are funded by the company that plans to obtain the marketing authorization.
In addition to clinical trials funded by pharmaceutical companies, investigator-initiated clinical trials are allowed, for which research grants are often provided by national centers.
3. What are the requirements for preclinical and clinical trial protocols? Who must approve the protocols?
There is no official requirement for preclinical trial protocols, but they have to comply with Japan GLP.
Clinical trial protocols must be submitted to the PMDA. Official approval is not required, but the PMDA will review and check the documents at the time of submission.
4. What are the requirements for consent by participants in clinical trials?
The investigator must obtain written consent from the participants. Before obtaining the written consent, the investigator has to provide written information to the participants, which must include information specified in the GCP rules, including the purpose of the clinical trial, the name and access information of the investigator, methods used in the clinical trial, possible adverse events, and trial compensation.
5. May participants in clinical trials be compensated?
Yes. The participants are paid a reasonable amount to compensate them for the burden of participation. Also, for patient participants, other medical expenses related to the clinical trial are paid by the sponsor.
6. How are participants in clinical trials protected and indemnified against any harm that arises as a result of participation in the trial?
The sponsor of the clinical trial is obligated to compensate participants for medical expenses, and to provide a medical allowance and compensation, and also has to prepare for such payments, including obtaining insurance.
Click the following links to read more legal articles from Japan:
- Regulatory Pricing and Reimbursement Overview
- Preclinical and Clinical Trial Requirements
- Marketing, Manufacturing, Packaging & Labeling, Advertising
- Traditional Medicines and OTC Products
- Product Liability
- Patents & Trademarks
- Regulatory Reform
Also from this Legal Handbook
11. Regulatory, Pricing and Reimbursement: Japan
An intro to the legal situation for regulatory, pricing and reimbursement in Japan. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
1. What are the regulatory authorities with jurisdiction over drugs, biologicals, and medical devices in your country?
The Ministry of Health, Labour and Welfare (the “MHLW”) and the Pharmaceuticals and Medical Devices Agency (the “PMDA”).
2. What is the regulatory framework for the authorization, pricing, and reimbursement of drugs, biologicals, and medical devices?
Authorization is governed by the Pharmaceuticals and Medical Devices Law (the “PMD Act”) of Japan.
Pricing of drugs and biologicals is governed by the National Health Insurance. Drug Pricing Standards are established by the MHLW under the Health Insurance Act. The method of calculation of drug pricing and the price of each drug are announced by the MHLW after consultation with the Central Social Insurance Medical Council.
Pricing of medical devices is included in the Medical Fee, which is also established by the MHLW under the Health Insurance Act, and the calculation method and price thereof are announced by the MHLW after consultation with the Central Social Insurance Medical Council.
Reimbursement is governed by the Health Insurance Act.
3. What are the steps to obtain authorization to develop, test, and market a product?
To develop and test a product, it is necessary to obtain a manufacturing/marketing business license depending on the type of business.
To market a product, in addition to the above, the license holder must obtain marketing authorization for each product.
4. What are the approximate fees for each authorization?
The fee for a manufacturing/marketing license varies depending on the type of license, but is approximately 100,000 to 150,000 yen. The fee for marketing authorization for each product varies depending on the product.
5. For how long are marketing authorizations/registrations valid? How are marketing authorizations/registrations renewed?
Manufacturing/marketing licenses are valid for five years, and the license holder must renew the relevant license(s) every five years. Marketing authorizations are valid until and unless withdrawn by the government for appropriate reasons or abandoned by the authorization holder, both of which are rare.
6. How does the authorization process differ between brand-name products and generic products? Are there differences for local manufacturers versus foreign-owned manufacturers?
Clinical trial data is required to obtain authorization for brand-name products. Normally, product creators spend more than 10 years from basic research to obtaining authorization.
For generic products, only stability tests and bioequivalence tests are required, as opposed to clinical trials. Thus, generic products can obtain authorization in a short time, normally 2 years from the start of testing. Currently, applications for authorization of generic products are accepted only twice a year, in February and August.
7. How are combination products (drug + drug, drug + biologic, drug + device, biologic + device, drug + biologic + device) regulated?
Basically, the same rules apply to combination products. To ensure the safety of combination products, the single drugs used in combination products must be in the market for one year or more, with exceptions for some special combination products (such as HIV drugs).
8. How is compliance with regulation monitored and evaluated? Is the regulatory regime comparable with the U.S. Food and Drug Administration or the European Medicines Agency expectations and requirements?
Compliance with regulations is monitored and evaluated by the PMDA and the local government of each prefecture. Basically, compliance with regulations is harmonized with the FDA and EMA.
9. What is the potential range of penalties for noncompliance?
Potential penalties include suspension of part or all of a business, cancellation of authorizations, or up to 3 years imprisonment or a fine of up to 3 million yen or both, depending on the type of noncompliance/misconduct.
10. Is there a national healthcare system? If so, how is it administered and funded?
There is a national healthcare system. Japan’s universal insurance system began with introduction of the Health Insurance Act in 1961. This system ensures that all people’s healthcare costs are covered by public insurance and that people have free access to any healthcare provider. People have to pay insurance fees to the health insurance program they join, and then, when the individual goes to a healthcare provider, the cost is covered by the National Health Insurance (other than a portion the individual patient must pay). The portion an individual must pay varies from 10% to 30% depending on the individual’s age; in addition, if an individual’s total payments exceed a certain amount, which is decided based on his or her income, the residual amount is covered by the National Health Insurance.
People have an obligation to join a health insurance program. Company employees join the health insurance program their employer has joined. Most other people join the national health insurance program, although there are also several special insurance programs such as the public employee union program.
The national healthcare system is funded primarily by insurance fees paid by the program members. For example, a company employee has an obligation to pay half of his/her insurance fee to the insurance program; the other half is paid by the employer. However, current healthcare costs are far beyond the total of insurance fees. Thus, there is an added public expense. Most recently, approximately one half of the total healthcare costs was covered by insurance fees, approximately 40% was covered as a public expense, and approximately 10% was covered by individual payment by the patients.
11. How does the government (or public) healthcare system function with private sector healthcare?
Most of the hospitals in Japan belong to the private sector (approximately 80%).
The basic functions of public sector and private sector hospitals are the same, but public sector providers have special missions, such as providing healthcare in remote places where no other hospitals exist, assisting patients as a safety net, and providing advanced healthcare based on advanced research and study.
12. Are prices of drugs and devices regulated and, if so, how?
Prices of drugs and devices are regulated under the Health Insurance Act.
Pricing of drugs and biologicals is governed by the National Health Insurance Drug Pricing Standard which is regulated by the MHLW under the Health Insurance Act. The methods of calculation of drug pricing and the prices for each drug are announced by the MHLW after consultation with the Central Social Insurance Medical Council.
The pricing of medical devices is included in the Medical Fee, which is also regulated by the MHLW under the Health Insurance Act, and the calculation methods and prices thereof are announced by the MHLW after consultation with the Central Social Insurance Medical Council.
13. How are drugs and devices used by patients paid for? What roles do public and private payers play?
Drugs and devices prescribed by doctors and used by patients are covered by the National Health Insurance, other than the portion individual patients must pay under the Health Insurance Act.
14. Who dispenses drugs and devices to patients and how are those dispensers compensated?
Doctors prescribe the drugs and pharmacies dispense the drugs to patients. When a pharmacy dispenses a prescribed drug, the patient has to pay a portion of the total cost, and the other portion is reimbursed to the pharmacy by the National Health Insurance payer.
The cost of devices used by doctors for patients is reimbursed to the doctor by the National Health Insurance payer. Patients only pay the hospital a portion of the doctor fees, including service fees.
15. What are the professional and legal responsibilities of those who dispense drugs and devices? What role do they play in providing patient care, information, and safety?
Under the Health Insurance Act, a doctor must register as an insurance doctor. Only registered insurance doctors can prescribe drugs and dispense devices covered under the national insurance system.
Also, only a pharmacy that is designated as an insurance pharmacy under the Health Insurance Act can dispense drugs.
Insurance doctors and insurance pharmacies have obligations under the Health Insurance Act, and non-compliance may result in cancellation of their licenses.
Click the following links to read more legal articles from Japan: