The Pharma Legal Handbook: Japan
 The Pharma Legal Handbook: Japan answers essential questions about the legal and regulatory environment for pharmaceuticals in Japan. It is a must-have for any company operating in the country or looking to enter the market.
The Pharma Legal Handbook: Japan answers essential questions about the legal and regulatory environment for pharmaceuticals in Japan. It is a must-have for any company operating in the country or looking to enter the market.
Prepared in association with Nishimura & Asahi, the largest international law firm in Japan, it should answer any questions linked to regulation, pricing, clinical and preclinical trials, marketing, manufacturing, trademarks and patents.
February 2022
1. Biosimilars & Biologics: Japan
The key facts about biosimilars and biologics in Japan. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here.
1. Are biosimilar medicines considered the same as generic medicines in your country?
A biosimilar medicine is differentiated from a generic medicine to the extent that final biosimilar products may differ from the original product, depending on the manufacturing process. This is because the production of biosimilars is much more complicated, due to the complex molecular structure and unique manufacturing processes for biopharmaceuticals; on the other hand, producing generic medicines is not difficult because ordinary pharmaceuticals have simple and stable low-molecular compounds. This means an authorization for biosimilars does not constitute evidence of pharmaceutical equivalence, bioequivalence, or clinical equivalence to the original (preceding) biopharmaceuticals.
2. Are all biologic medicines, including biosimilar medicines, patentable in your country?
Yes, as long as the biologic medicine meets the general requirements of the Patent Act, its patentability is assured; in Japan, the patentability of biologic medicines is not specifically provided for in the act and other laws.
In this regard, Japan has not yet established a statutory system that coordinates the relationship between market approval for generic medicines or biosimilar medicines and the patent status of their branded original, such as a patent linkage system provided in the Drug Price Competition and Patent Term Restoration Act (well known as the Hatch-Waxman Act) or a patent dance system provided in the Biologics Price Competition and Innovation Act of 2009 (the “BPCIA”) in the United States. Though, as for generic medicines, a similar system has been put into practice at the governmental notification level. Under this coordination system, companies cannot obtain marketing approval for a generic medicine prior to the expiration of the patent term on the branded equivalent.
However, it is uncertain whether the word “generic medicine” in the notification includes biosimilar medicines. This suggests that it is possible that biosimilar medicines will not be treated in the same way as generic medicines, resulting in a situation where biosimilar medicines cannot acquire linkage protection. Therefore, the situation surrounding the patentability of biologic medicines is significantly different from other countries which have particular biopharmaceutical-protection systems, such as the BPCIA in the United States.
3. Is there a specific regulatory framework for the marketing authorization of biosimilar medicines in your country? If yes, what is the regulatory framework for the authorization of biosimilar medicines?
No. Refer to Question 2 with regard to the relationship between market approval for a biosimilar medicine and the patent status of its branded original.
4. What kind of data package is needed to obtain approval for a biosimilar drug? Is this any different to the requirements for the original Biologics drug?
Under the PMD Act, which establishes the need for market approval, there is no difference between the approval requirements for biosimilar drugs and those for other drugs. However, in many cases, it is difficult to prove that the active ingredients in the original Biologics drug are identical to those in its biosimilars, so it is thought that the same approval approach used for generic products cannot be applied to biosimilars.
Given this situation, the MHLW specifically issued a notification and guideline for market approvals for biosimilars. According to this documentation, the essential data required to obtain approval for a biosimilar drug are (1) data detailing the origin or history of discovery and usage status in foreign countries; (2) data detailing the manufacturing method, standards, test methods, etc.; (3) data detailing stability; (4) data detailing pharmacological action; (5) data detailing toxicity; and (6) data detailing the results of clinical studies. In addition to these data, depending on the nature of the biosimilar product, other data may be required.
5. What are the requirements for the choice of the reference comparator product?
According to the MHLW’s guideline, the reference product to which a biosimilar should be compared is a biologic drug that has been already authorized on the basis of a complete data package in Japan. Another biosimilar can never be used as a reference product, throughout the entire duration of the biosimilar development period (including the quality development period, non-clinical development period, and clinical development period).
6. Can the comparator product be sourced from another regulatory jurisdiction? If yes, what are the data needed to support this approach?
No. As mentioned in the response to Question 5, under the MHLW’s guideline, the reference comparator product must be a drug already authorized in Japan.
7. How are the prices of biosimilar medicines regulated? Is this any different from the requirements for the original Biologics drug?
In Japan, it is typically expected that drugs will be used under the auspices of the national health insurance system. The Japanese government determines the price of medicines by using a model established pursuant to the national health insurance pricing system.
The price of a new biosimilar medicine is generally determined by multiplying the standard price (which is calculated based on the price of the most similar drug to the biosimilar medicine) by 70%. However, for internal medicines, when the brand number of the same kind of biosimilar product (limited to those with similar efficacy and effect to the new biosimilar product) exceeds 10, the new biosimilar medicine’s price is determined by multiplying the standard price (as calculated the same above) by 60%. Exceptionally, based on the results of clinical trials, it may be possible to add a 10% premium (at most) to the price of a new biosimilar medicine.
8. What is the reimbursement policy for biosimilar medicine? Is this any different from the requirements for the original Biologic drug?
Biosimilar medicines are reimbursed under the National Health Insurance system in the same manner as other drugs. There is no special reimbursement procedure for biosimilar medicines.
In this regard, the Japanese government has promoted the development and use of biosimilars, and introduced special treatment regarding self-injection of biosimilars by patients, under which a certain price is added to self-injection instruction management charges when biosimilars are prescribed with the patient’s consent. Please note that this treatment is one kind of reimbursement (medical fee) revision under the National Health Insurance system, notwithstanding the medicine price decision itself, based on the PMD Act. This treatment has been in force since April 1, 2020.
9. Does biosimilar competition impact the reimbursement policy of the originator reference products?
Yes. The Japanese government has promoted biosimilars, which means there may be a strong competitive effect on the existing biopharmaceuticals market. This is mainly due to the fact that they are less expensive (as mentioned in the response to Question 7) and in light of the reimbursement policies (as mentioned in the response to Question 8). The Japanese government is planning other strategies to accelerate the introduction of biosimilars into medical practice in Japan, so it is necessary to continue monitoring these movements.
10. What is the legal framework for biosimilar medicines prescribing (clinical decision maker) and dispensing (pharmacy level, hospital or retail)? Is this any different to the requirements for the original Biologics drug?
There is no particular legal framework for prescribing biosimilars.
11. Is the system considering physician-led switching and/or pharmacy-level substitution (without involvement of the clinical decision maker)?
Switching patients from biologics to biosimilars is fundamentally permitted for doctors. There is no clear rule banning pharmacists from changing biologics to biosimilars, but it is not recommended that pharmacists do so, in medical practice.
12. What are the post – authorisation requirements (including pharmacovigilance, risk management plans, post-approval studies) for biosimilar medicines? Is this any different to the requirements for the original Biologics drug?
Manufacturers must set up methods for post-marketing safety control for pharmaceuticals (referring to collecting and reviewing matters related to quality, efficacy and safety, and other information necessary for the appropriate use thereof, and necessary measures based on the results), and those methods have to comply with the standards specified by order of the MHLW. This rule also applies to biosimilar medicines, but if their efficacy and safety are assured by the original biologics drugs, they are exempt from this rule, including post-marketing safety control research.
However, a guideline by the MHLW (referred to in the response to Q126) suggests that manufacturers should research the safety profiles of biosimilar medicines. In terms of this post-marketing safety control research, the guideline also requires that manufacturers anticipate risks that could not be sufficiently evaluated by the equivalence/homogeneity evaluation during the development stage, formulate an appropriately designed post-marketing surveillance plan based on those risks, and submit it to the authority when applying for approval. In addition, the guideline provides that the results of such a post-marketing surveillance plan should be delivered to the authority by the appropriate time after approval of the biosimilars.
13. Are there specific policies and requirements for labelling biosimilar medicines in the event of second medical use patents? Is this any different from the requirements for the original Biologic drug?
No. There are no specific policies and requirements regarding the labelling of biosimilar drugs in the case of a second medical use patent.
14. Have there been any significant legal/judicial developments in relation to biosimilars in your country? (Including but not limited to IP, procurement, competition, misleading information campaign, access to reference comparator product)
Yes. In recent years, the Japanese government has promoted biosimilars in some way. Please refer to Question 7 and Question 9.
15. Are there proposals for reform or significant change to the legal, regulatory, procurement of biosimilars? If yes, when are they likely to come into force?
Yes. In recent years, the Japanese government has promoted biosimilars in some way. Please refer to Question 7 and Question 9.
————————————————-
- The the Minister of Health, Labour and Welfare (“MHLW”) as the Japanese authority issued a notification detailing this matter: https://www.mhlw.go.jp/web/t_doc?dataId=00tb5511&dataType=1&pageNo=1
- http://www.nihs.go.jp/dbcb/TEXT/yakusyokuhatu-0304004.pdf
https://www.pmda.go.jp/files/000206248.pdf -
Please refer to the detailed calculation method; online: https://www.mhlw.go.jp/content/000497468.pdf
Also from this Legal Handbook
2. Localization: Japan
The key facts about localization in Japan. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
1. Are there any rules or regulations requiring and/or encouraging localization in your country? What is the legal framework defining these localization rules and policies?
No, there are no rules or regulations requiring and/or encouraging localization in Japan. This means that the decision about whether to import and sell pharmaceuticals made in foreign countries or to sell domestically manufactured pharmaceuticals generally is left to the distributors’ individual judgment.
Please note that no person other than one who has obtained marketing authorisation from the MHLW may engage in the business of marketing pharmaceuticals in Japan. This regulation is set forth in the PMD Act. In relation to obtaining such a license, this law requires that the applicant should have methods for quality control for pharmaceuticals which comply with the standards specified by the Order of the MHLW for the purpose of obtaining such license; one such order is the Ministerial Ordinance on Standards for Quality Assurance for Drugs, Quasi-drugs, Cosmetics and Medical Devices. According to this order, a marketing authorisation holder shall have a person, designated beforehand, in its quality assurance department or manufacturing department who evaluates the results of the manufacturing control and quality control and makes decisions concerning the market release for each lot. This rule applies to distributors (marketing authorisation holders) who sell pharmaceuticals imported from foreign countries.
2. Have there been any recent significant changes involving localization rules? If yes, when did they take place and what did they involve?
N/A.
3. Is the process of obtaining a marketing authorization impacted by localization policies in your country? If yes, how so (what are the incentives received or the requirements)?
N/A.
4. Is the pricing process for pharmaceutical products impacted by localization policies in your country? If yes, how so (what are the incentives received or the requirements)?
N/A.
5. Is the reimbursement of pharmaceutical products impacted by localization policies in your country? If yes, how so (what are the incentives received or the requirements)?
N/A.
6. Is the access to public or public tenders of pharmaceutical products impacted by localization policies in your country? If yes, how so (what are the incentives received or the requirements)?
N/A
7. Are import tariffs, importation and/or exportation permits, trade and/or taxation of pharmaceutical products impacted by localization policies in your country? If yes, how so?
N/A.
8. Are there any other incentives or advantages offered by the current local localization rules in your country? If yes, what are they?
N/A.
9. Are there discussions about the possibility of implementing localization policies in your country? If yes, what are the proposed reforms and when should they come into place?
Currently, there are no discussions in progress concerning the possibility of implementing localization policies in Japan.
Also from this Legal Handbook
3. Cannabinoid Drugs, Medicinal Cannabis and Opioid Drugs: Japan
Keen to learn more about cannabinoid drugs, medicinal cannabis and opioid drugs in Japan? Read on! Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
Cannabinoid Drugs
1. Are Cannabinoid Drugs authorized in your country?
No. In Japan, the utilisation of cannabis (all kinds) is severely restricted by two acts.
The first is the Cannabis Control Act, under which “Cannabis” is defined as the cannabis plant (Cannabis Sativa L.) and its products; provided, however, that the grown stalk of the cannabis plant and its products (excluding resin) and the seed of the cannabis plant and its products are excluded from this definition. The Cannabis Control Act states that any person who is not a cannabis handler (the term “cannabis handler” includes cannabis researchers) must not possess, cultivate, receive, or transfer cannabis, or make research use of it. Furthermore, it is prohibited for any person to perform any treatment with medicines manufactured from cannabis, to distribute cannabis for treatment purposes, and/or to receive treatment with any medicines manufactured from cannabis.
It is worth noting that this act does not prohibit the act of using cannabis (including the act of smoking cannabis) per se. This is due to the fact that before World War II, cannabis grass was widely cultivated in Japan, and even today cannabis grass is grown in some parts of Japan for its fibre, which is used in clothing; this leads to the possibility that farmers accidentally might inhale cannabis components dispersed into the air when they cut cannabis grass.
The second act is the Narcotics and Psychotropics Control Act. This Act aims to prevent any health and sanitation hazards caused by the abuse of narcotics (and psychotropics). Cannabis is not expressly covered in the act, but tetrahydrocannabinol (THC), a major cannabinoid present in cannabis, is regulated as a narcotic under the act, provided it is chemically synthesized.
2. What are the regulatory authorities with jurisdiction over Cannabinoid Drugs?
N/A.
3. Is there a specific regulatory framework for the authorization, pricing, and reimbursement of Cannabinoid Drugs?
N/A.
4. Which are the cannabinoid drugs that have received market approval to date?
N/A.
5. Who can prescribe Cannabinoid Drugs?
N/A.
6. Is there a list of doctors authorized to prescribe Cannabinoid Drugs?
N/A.
7. What approvals or notifications are required to prescribe Cannabinoid Drugs?
N/A.
8. Which organizations are authorized to sell/distribute Cannabinoid Drugs available?
N/A.
9. Is there a list of retailers/distributors authorized to sell Cannabinoid Drugs?
N/A.
10. Are there proposals for reform or significant change to the regulation of Cannabinoid Drugs?
In June 2021, after considering the recent trends in other countries and the medical usefulness of cannabis, a study council organised by the MHLW proposed that the production and application of medicines made from cannabis should be made possible.
11. When are they likely to come into force?
Despite the aforementioned proposal, at present there is no active debate in the Japanese Parliament concerning the production and sale of cannabis-based medicines.
Medicinal Cannabis
12. Is Medicinal Cannabis authorized in the country?
Any use of all types of cannabis is banned by the Cannabis Control Act, regardless of the name of the product or the purpose of its use, unless it is made from grown stalks or seeds of the cannabis plant (refer to Q68). One notable exception is cannabis researchers (persons who receive licenses from a prefectural governor and cultivate cannabis plants for the purpose of researching cannabis). Cannabis researchers are permitted to possess, cultivate, receive, and/or transfer cannabis, and to make research use of it. Additionally, cannabis researchers are allowed to import cannabis to Japan only if they satisfy certain requirements (refer to Q82).
13. What are the regulatory authorities with jurisdiction over Medicinal Cannabis?
N/A.
14. What is the regulatory framework for the authorization, pricing, and reimbursement of Medicinal Cannabis?
N/A.
15. How is the production and import of Medicinal Cannabis regulated and by which agencies/authorities?
Under the Cannabis Control Act, the import of cannabis to Japan is prohibited. However, cannabis researchers who have received authorisation from the MHLW to import cannabis are excluded from this prohibition.
16. What approval or notifications are necessary to produce or import Medicinal Cannabis?
Registration as a cannabis researcher is the first requirement. Moreover, to import cannabis, it is also necessary for the relevant cannabis researchers to receive authorization from the MHLW.
17. What is the regulatory framework for the marketing and distribution of Medicinal Cannabis?
N/A.
18. How can patients obtain Medicinal Cannabis?
N/A.
19. Who can prescribe Medicinal Cannabis?
N/A.
20. Is there a list of doctors authorized to prescribe Medicinal Cannabis?
N/A.
21. What approvals or notifications are required to prescribe Medicinal Cannabis?
N/A.
22. Where is Medicinal Cannabis available?
N/A.
23. Is there a list of retailers authorized to sell Medicinal Cannabis?
N/A.
24. Are there proposals for reform or significant change to the regulation of Medicinal Cannabis?
N/A.
Opioid Drugs
25. Are Opioid Drugs authorized in your country?
Some Opioid Drugs are authorized for sale as legitimate pharmaceutical products, based on the PMD Act. Additionally, in Japan, most opioid drugs are treated as narcotics and regulated under the Narcotics and Psychotropics Control Act. Therefore, as long as the requirements are satisfied, Opioid Drugs may be medically prescribed and distributed in compliance with the stringent regulatory framework established by those acts and the related regulations.
26. What are the regulatory authorities with jurisdiction over Opioid Drugs?
The central authority with jurisdiction over Opioid Drugs is the MHLW. Prefectural governors and the heads of the respective Regional Bureaus of Health and Welfare are also involved in issuing some licenses.
27. Is there a specific regulatory framework for the authorization, pricing, and reimbursement of Opioid Drugs?
Opioid Drugs can be authorized for sale in Japan once the relevant review process has been completed successfully, in accordance with the applicable requirements in the PMD Act and related regulations.
There is no specific regulatory framework for the pricing of and reimbursement for Opioid Drugs in Japan.
28. Which are the Opioid drugs that have received market approval to date?
Some Opioid Drugs already have received market approval. They include morphine, oxycodone, fentanyl, methadone, hydromorphone, codeine, and dihydrocodeine. Please note that these Opioid Drugs are designated as narcotics under the Narcotics and Psychotropics Control Act.
29. Who can prescribe Opioid Drugs?
Essentially, it is prohibited for anyone who is not a Person Licensed to Administer Narcotics to administer a narcotic, deliver a person a narcotic to administer, or deliver a prescription for a narcotic. A “Person Licensed to Administer Narcotics” means a person who has been licensed by the prefectural governor to administer narcotics, deliver a person a narcotic to administer, or deliver prescriptions for a narcotic in the course of business and as treatment for an illness. It is not permissible for a person other than a physician, dentist, or veterinarian to obtain licensing as a Person Licensed to Administer Narcotics.
30. Is there a list of entities authorized to prescribe Opioid Drugs?
No. There is no public list of licensed doctors authorized to prescribe Opioid Drugs as a Person Licensed to Administer Narcotics in Japan.
31. What approvals or notifications are required to prescribe Opioid Drugs?
Persons Licensed to Administer Narcotics may prescribe Opioid Drugs without additional approval or notification. Please note that a Person Licensed to Administer Narcotics must not administer a narcotic, deliver a narcotic to administer, or deliver a prescription for a narcotic for any purpose other than treatment for an illness.
32. Which organizations are authorized to sell/distribute Opioid Drugs available?
Essentially, it is prohibited for anyone who is not a Commercial Narcotics Handler to sell/distribute a narcotic. A “Commercial Narcotics Handler” means a Narcotics Importer, Narcotics Exporter, Narcotics Manufacturer, Formulator of Narcotic Pharmaceuticals, Manufacturer of Exempt Narcotics, Primary Wholesaler of Narcotics, Narcotics Wholesaler, or Narcotics Retailer.
33. Is there a list of retailers/distributors authorized to sell Opioid Drugs?
No. There is no public list of licensed retailers/distributors authorized to sell Opioid Drugs in Japan.
34. Are there proposals for reform or significant change to the regulation of Opioid Drugs?
No. There is currently no noticeable movement for reform of or significant changes to the regulation of Opioid Drugs.
35. When are they likely to come into force?
N/A.
Also from this Legal Handbook
4. Orphan Drugs & Rare Diseases: Japan
The ins and outs of orphan drugs & rare diseases in Japan. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
1. What is the definition of Rare Diseases in your country?
In Japan, there is no fixed definition for Rare Diseases, although the concept is included in the definition of Orphan Drugs (refer to Q104). It should be noted that our country has a system to deal with diseases designated as “Intractable Diseases,” the definition of which is provided in the Act on Medical Care for Intractable Disease Patient (the “Intractable Disease Act”), but the range and definition of Rare Diseases do not necessarily correspond to those of Intractable Diseases.
2. Does the designation of ‘Orphan Drug’ exist in your country? (Does it correspond with the definition of Rare Diseases?)
An “Orphan Drug” is defined as a pharmaceutical designated as such by the MHLW under the PMD Act. More specifically, the MHLW can designate a pharmaceutical as an Orphan Drug when all of the following requirements are satisfied: (i) the number of patients who need the drug is less than 50,000; (ii) there is no alternative drug, and the drug has particularly excellent efficacy or safety; and (iii) the manufacturers have a possible and reasonable development plan for the drug. As an exception to requirement (i), if a disease falls within a category provided in the Intractable Disease Act, the number of patients may be changed to comply with the relevant provision of that act.
3. What is the regulatory framework for the authorization of an Orphan Drug? (Is this regulatory framework based on Rare Disease status or can it alternatively be based on Orphan Drug foreign status?)
Designation of an Orphan Drug does not immediately lead to approval (authorization) for the manufacture and sale of the drug. The process for Orphan Drug authorization is essentially the same as that for ordinary drugs. However, certain priority treatment is given during the approval review for an Orphan Drug, for purposes of expediting its development. More precisely, if a drug is designated as an Orphan Drug, its approval review is prioritized (in terms of time) over an examination or investigation into other pharmaceuticals. The Japanese regulatory framework does not consider an Orphan Drug’s foreign status.
4. Does your country have provisions for relaxed clinical trial/scientific evidence requirements in respect of Orphan Drugs as compared to other drugs?
No. Currently, Japan does not have any provisions for relaxed clinical trial/scientific evidence requirements with respect to Orphan Drugs as compared with other drugs.
5. Is there an expedited pathway for Orphan Drugs?
As stated in Q104, if a drug is designated as an Orphan Drug, a priority review process is applicable to the approval (authorization) of the manufacture and sale of the drug. To clarify, however, there is no expedited pathway for the designation of Orphan Drugs.
6. Are foreign marketing authorizations recognized in your jurisdiction for Orphan Drugs? If yes, marketing authorizations from which countries are recognized?
No foreign marketing authorizations are recognized for Orphan Drugs in Japan.
7. Can Orphan Drugs be reimbursed? If so, is there a specific reimbursement procedure for Orphan drugs?
Yes, Orphan Drugs are reimbursed under the National Health Insurance. However, there is no special reimbursement procedure for Orphan Drugs.
8. How are the prices of Orphan Drugs regulated?
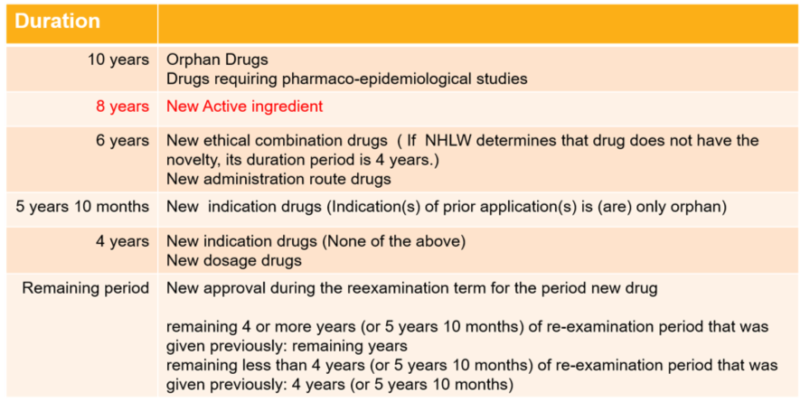
In Japan, drugs are typically expected to be used under the auspices of the national health insurance system. The Japanese government determines the price of medicines by using a model established under the national health insurance pricing system. The prices of Orphan Drugs are regulated in the same manner as other drugs. However, under the pricing model, Orphan Drugs will normally receive an additional price. In addition, Orphan Drugs receive special treatment regarding price decisions, under which the prices of Orphan Drugs are exempt from periodic price cuts for a certain period of time.
9. In case of reference price based on a basket of countries, what countries are included?
When determining the price of a new drug that already been made available for sale in countries other than Japan, the government adjusts the price so that there is no significant price difference between Japan and certain other countries. The countries used for comparison are the United States, the United Kingdom, Germany, and France.
10. Have there been any significant legal/judicial developments in relation to Orphan Drugs in your country?
No. There have not been any recent significant legal/judicial developments relating to Orphan Drugs in Japan.
11. Are there proposals for reform or significant change to the regulation of Orphan Drugs? If yes, when are they likely to come into force?
No. There is currently no noticeable movement for reform of or significant changes to the regulation of Orphan Drugs.
Also from this Legal Handbook
5. Regulatory Reforms: Japan
The key facts about regulatory reforms in Japanese Pharma. Prepared in association with Nishimura & Asahi, a leading law firm in Japan, this is an extract from The Pharma Legal Handbook: Japan, available to purchase here for GBP 149.
1. Are there proposals for reform or significant change to the healthcare system?
No proposal is pending for significant reform or change to the healthcare system in Japan. However, there are small changes every year. For example, there have been changes due to technology, telemedicine, apps as a medical device, and enactment of the Healthcare Big Data Act, and changes due to compliance issues, promotion guidelines, monitoring, and enactment of the Clinical Trials Act.
2. When are they likely to come into force?
Small changes and developments occur on an ongoing basis.
Click the following links to read more legal articles from Japan:
- Regulatory Pricing and Reimbursement Overview
- Preclinical and Clinical Trial Requirements
- Marketing, Manufacturing, Packaging & Labeling, Advertising
- Traditional Medicines and OTC Products
- Product Liability
- Patents & Trademarks
- Regulatory Reform